Can GnRH analogues reverse autistic perimenopausal regression in one month?*
The initial effects of GnRH analogue implants on two PDAuDHD** midlife women
* Nope
** PDAuDHD stands for pathological demand avoidant/pervasive drive for autonomy (PDA) profile autistic with co-occuring attention deficit hyperactive disorder (ADHD)
⚠️ Content warning: this article mentions suicidal ideation, which can be a symptom of autistic hormonal depression and peri/menopause. Please take care if you decide to read it, and reach out for urgent help if you are experiencing suicidal thoughts. ⚠️

💕“Wishing you luck for Wednesday. We should have a little (virtual) menopause party, you and I! It feels like such a such a big moment in a strange way… We are fellow guinea pigs!” 💕said my new friend Emma***, 36, two days before my GnRH analogues implant.
*** Real name changed for privacy. Emma has kindly given me permission to share her story, and has checked the content for accuracy. She is two weeks ahead of me in the same treatment used to stop extreme hormonal fluctuations.
Well, this past month has certainly been a treacherous ride, and one I am not sure I would have coped with alone. The first month of GnRH analogues treatment has not been the cure all I had hoped for when I have written about it previously…
I have been plunged back into severe menopausal symptoms, with my morose mood driving my energy lower and lower. Or perhaps my low energy is driving my deteriorating mental health? Either way, I am not having the graceful and inspo-worthy post-menopause renaissance so many neurotypical celebs and influencers are raving about in mainstream media.
I do not feel reborn, in fact, I feel much closer to death than to a revival.
Late diagnosed autistics need neuro-affirming communication, community, companionship and skilled healthcare professionals
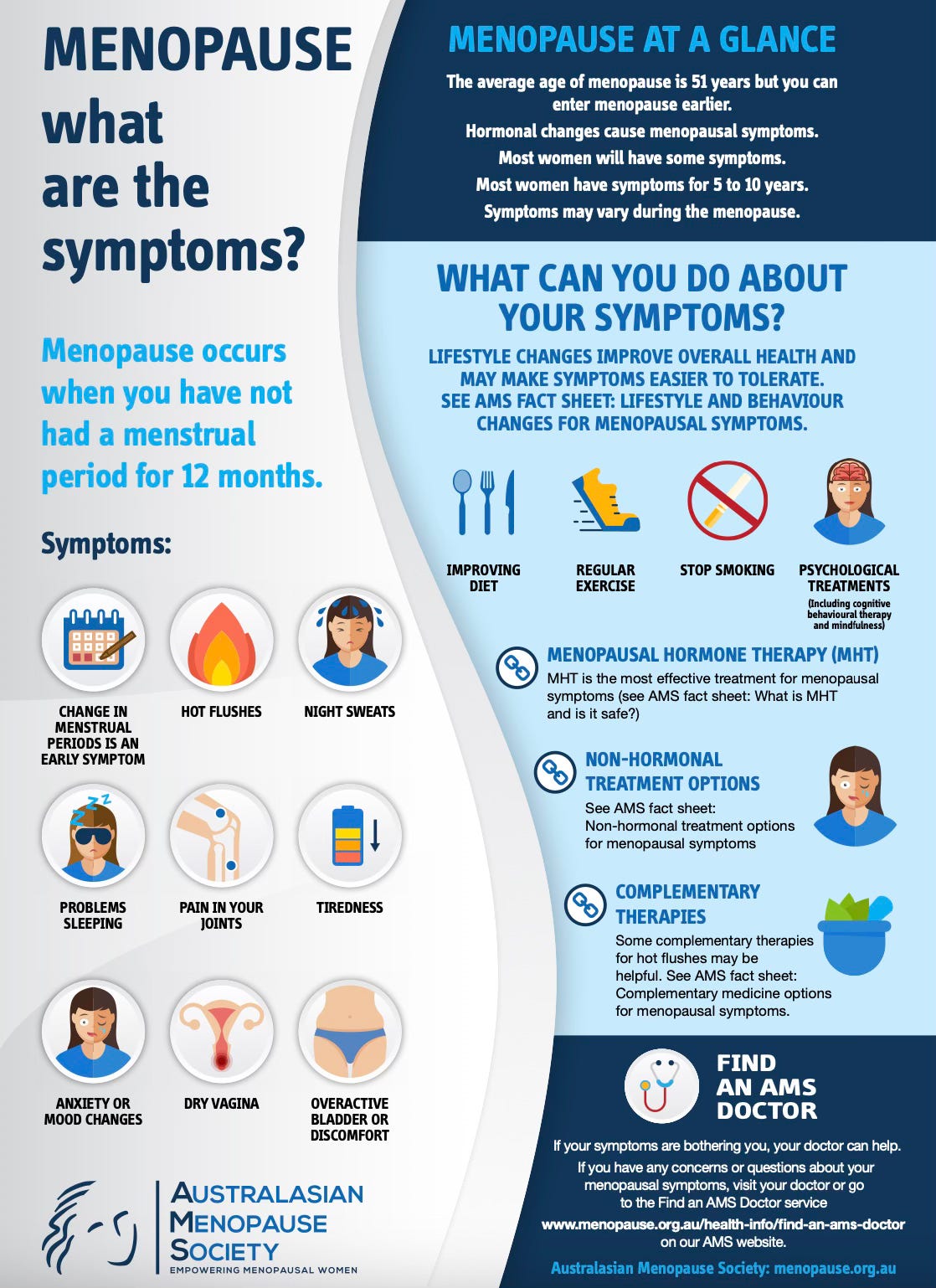
Autistic perimenopause can start earlier than in the average population. Emma is 36 years of age, and I am 43. The average age of menopause is 51 (according to the Australasian Menopause Society website). Emma and I share the same neurodevelopmental conditions of PDAuDHD, so we have similar communication styles that are not at all like those of neurotypicals. We can jump in and out of a Facebook Messenger text conversation without wasting our finite capacity on social niceties and small talk.
Our initial online connection moved quickly from innocent Ragdoll pet cat photo swaps to “Oh, we are both autistic and seeing the same HRT doctor!”
Emma and I are lucky to have found our doctor. Our HRT doctor is amazing, and one of a kind here in Aotearoa New Zealand. Not only does she have up to date medical knowledge on treating people through their menopausal transition, but she also has a neuro-affirming medical practice, delivering expert female general practitioner (GP/family doctor) care both in person and remotely through Telehealth via phone, emails and the MyIndici 2.0 app medical doctor/patient communication portal. She uses visuals and graphic information, takes time to explain treatment options, and knows to give her neurodivergent patients additional information processing time. This is vital, as we are then empowered to make our own treatment decisions. We can go away and listen to podcasts, seek information from other reputable sources, discuss with our partners/friends/online peer groups, and return making a supported and informed decision. After decades of medical misogyny and medical gaslighting, she is genuinely wonderful.
Emma and I now have almost daily exchanges on our severe and sudden onset of post-GnRH analogues-induced menopause symptoms, whilst individually titrating our HRT doses under our doctor’s supervision, to optimise our oestrogen saturation with patches and pills, protect the womb lining from endometrial cancer using progesterone pills (orally or vaginally, depending on your doctor’s advice), plus my testosterone gel.
All of this whilst coping with a global shortage of oestrogen patches (that now seems to have resolved), and contemplating alternatives such as oestrogen gels or pills. It has been a precarious time for all of us.
As many of us are all too aware, life can be very isolating for late diagnosed autistic woman, and perhaps more so in midlife. Luckily for me, I have struck gold and found both an excellent doctor, and a new friendship in Emma, who is unfortunate enough to also be having an exceptionally shit time of perimenopause. Emma has confided in me that she has pre-menstrual dysphoria disorder (PMDD), and that the first month of the GnRH analogues virtually eliminated her usual PMDD symptoms.
In Emma’s own words:
“Yes, the PMDD became really severe as perimenopause advanced and no other first or second line treatments were working. I'd never heard of it before, but there was good information about it on this website which our doctor shared with me. It's proving to be life saving treatment for me. As someone who is no stranger to severe depression, the PMDD that came with perimenopause was actually terrifying and it was burning through every barrier I had between myself and going off the edge of the cliff. I knew I was in trouble and I'm extremely grateful my two doctors were willing to take the risk and supported me right through the process.
“There is a big risk that Zoladex can worsen depression, and I did struggle initially with getting the right HRT dose. I remember calling our doctor in a panic after I started pulling every lever I had between the estrogen patches and the Utrogestan (progesterone pills) since my new dose would need to change significantly and I couldn’t find the balance. It was like learning to drive a manual car all over again. Estrogen was the petrol pedal and Utrogestan, the clutch control. I was stalling all over the place. My doctor very calmly took the wheel for me and made sense of the muddle I was in and got me back on track.
“I don't know if GPs ever feel like they've saved lives in the course of their career, but my two certainly have saved mine.”
What is a chemical menopause?
The following is an excerpt from Dr Louise Newson’s Balance app/website article ‘Chemical menopause: what is it and what can I expect?’
“Some medications, including hormone blockers, can induce a temporary, but often more intense, menopause
Certain medications, such as those used to treat endometriosis and some types of cancer, can stop hormone production in your body
Symptoms of a chemical menopause can be similar to those in menopause but usually start more suddenly and can be more severe
Add-back HRT and testosterone can often be taken, which reduces menopausal symptoms and improves long-term health…
… These medications (e.g. Zoladex) “switch off” your hormones, meaning that the production of hormones oestrogen, progesterone and testosterone is stopped or reduced. This is usually temporary while you are given the medication and is usually reversible after you stop having the medication.”
The Zoladex procedure
My GnRH analogues implant (Zoladex) stung a bit at the injection site, and I developed a very impressive bruise, which I wasn’t afraid to show to anyone willing to take a peek. The one monthly dose implant (there are three month doses as an alternative after the initial trial) is the size of a grain of rice, injected into subcutaneous belly fat, of which I have plenty, thanks to perimenopause and my chronic chocolate habit. The implant dissolves as over the course of four weeks, releasing the GnRH analogues gradually, which switch off the ovaries. As I have no medical qualifications, I am going to stay in my own lane and let this video explain it:
As the month progressed, the bruise at the implant site went through the entire colour spectrum and, in the fourth week, finally faded out. The second implant has not bruised at all. It was uncomfortable having it injected on both occasions, but the first time was the worst, as I was acutely aware of the injection site for a couple of weeks afterwards. It was more of a scratchy poky discomfort than pain, and was exacerbated by the presence of a bruise the same dimensions as my computer mouse here beside me. 😖
Side effects of GnRH analogues are symptoms of menopause (PSA: they are not just a dry vagina, a lack of libido and hot flushes! In fact, you can have none of those symptoms and still be in perimenopause.)
During the first month of my chemical menopause, I have experienced:
Dry eyes and visual irritation
Constant bladder urgency and worry about bladder control issues
Cognitive regressions and working memory lapses
Decreased sleep duration and lower quality sleep
The Rage, irritability, frustration and short temperedness
Joint and muscle pain
Weakness in my hands and wrists
Constant lower back ache plus pelvic pain akin to menstrual cramps, minus the bleeding
Aversion to physical activity
Tired all the time
Dry, irritated, tight feeling skin
Hot flushes and inability to regulate my body temperature
Suicidal ideation, suicidal thoughts and worryingly dark moods
Health anxiety
Palpitations, heart beating strongly or quickly
Lightheadedness
Tinnitus (ringing or buzzing in the ear), and increased auditory processing overwhelm
Headaches
Weight gain, bloating and irritable bowel
Loss of interest in most things
Lack of patience and engagement with others
Dissociation from usual tasks and relationships
Lack of motivation and increased inertia
Hypersensitivity to sensory input such as clothing
Increased skin picking, nail biting, tics and pacing
Decreased concentration when driving
Inability to fulfil prior booked engagements
Regression in household care tasks such as meal preparation
Increased support needs in adulting
To bleed, or not to bleed: that is the question
Emma warned me around weeks two and three that:
“Your last period will be a shocker so please prepare very good pain relief in advance… I have had such severe pain I’ve been nauseous and clammy from the intensity of the cramping.”
Emma ended up visiting A&E for heavy bleeding and intense pain, but left before they discharged her because waiting rooms are often not psychologically safe spaces for distressed autistic people. It turned out to be a fibroid and an incredibly heavy bleed, and I braced myself for the worst.
Fortunately, my Mirena intrauterine device (IUD) which I had inserted a year ago due to constant bleeding, seems to have prevented my “final” period. I am someone optimistic that my final ever bleed was over two months ago, and was light although painful, seemingly triggered by the emotional distress of sitting at my Dad’s hospital deathbed. Unfortunately, the GnRH analogues have exacerbated my grief and low mood, and have triggered several episodes of suicidal ideation. At some points, I have just had to curl up on the sofa and wait them out, often under several weighted blankets, and attempting to sleep to block out the psychological distress and emotional pain.
💕 One dark stormy evening here in Aotearoa New Zealand’s late Winter during the second week of my autistic chemical menopause, I plunged into a fitful bout of sleep on the sofa. Somewhere between a fever dream and a hot flush, I dreamt that I had decided to end it all, and I was with my Dad. Expecting him to be glad to see me, he told me I had no place to be with him yet. That it was not my time, and my husband and young children need me here with them. I woke up in distress, but took this heart-wrenching message on board, got straight up, went to the kitchen and tried to make myself useful back here in my own life. 💕
My burgeoning dark mood has not yet lifted, and I have noticed a pattern of being at my worst in the late afternoon to early evening. I suspect this may be related to the time that my ADHD stimulant medication wears off, causing a medication rebound, AKA the Adderall crash, in symptoms. I am having to ride that out because I can only handle so many variables at once, and now is not a good time to lose the beneficial effects of stimulant medication for treating my executive functioning and emotional regulation. I can only extinguish one fire at a time, or at the very least, maintain the controlled burn that is my late diagnosed autistic midlife.
The Autistic Perimenopause is complex and multifaceted, but also misunderstood and underestimated
Emma and I are both holding out for eventual progressions with ongoing GnRH implants, to maintain our temporary, reversible and chemical menopauses. We are psychologically and emotionally safe with each other and our doctor, and will tell each other when we are experiencing dangerously low mood and/or suicidal thoughts. We also have husbands who are looking out for us, which admittedly is a safe and privileged position to be in.
Do you have a support plan in place for surviving low moods, menopausal depression and suicidality?
The Meno-D rating scale to detect depression in menopause is a useful tool you can use to share your current rating without needing to speak. The categories are low energy, paranoid thinking, irritability, self-esteem, isolation, anxiety, somatic symptoms, sleep disturbance, weight, sexual interest, memory and concentration.
What do you think we need in autistic perimenopause to support our transition? I’ll start us off, please add your thoughts in the comments.
💕 We need doctors and healthcare professionals who validate us, and are willing to look at us individually through a neuro-affirming lens.
💕 We need our mental health, wellbeing and distress taken seriously.
💕 We need to know about menopause symptoms in advance, and accept that this hormonal transition can cause temporary regressions to our functioning and capacity.
💕 We need companionship and community to survive this unavoidable life stage.
💕 We need robust medical information presented in graphic visuals, with alternative communication methods as appropriate to our individual needs.
💕 We need investment in academic research on the autistic menopausal transition in order to identify optimal information sharing, support and treatment.






Ps. My adhd meds seem to be making me even more tired lately and can’t counteract the fatigue 🙈
I’m nearly 45yo and feeling ready to board the HRT train. I recently had an ‘endometrial ablation’ to reduce heavy bleeding, so at least side of things is under control now (I said no to a Mirena as I hated the thought of having that inside me all the time!). But yeah - I’ve always struggled with PMDD, but lately I just feel so exhausted/weak/achy, have recurring headaches and low mood etc (most of the time) that I figure starting HRT is the logical next step. Here’s hoping it doesn’t negatively impact me like it did you AuDHD painter 🤞 (I’m sorry this was your experience).
Thanks for all your posts Sam…they’re really helpful ☺️