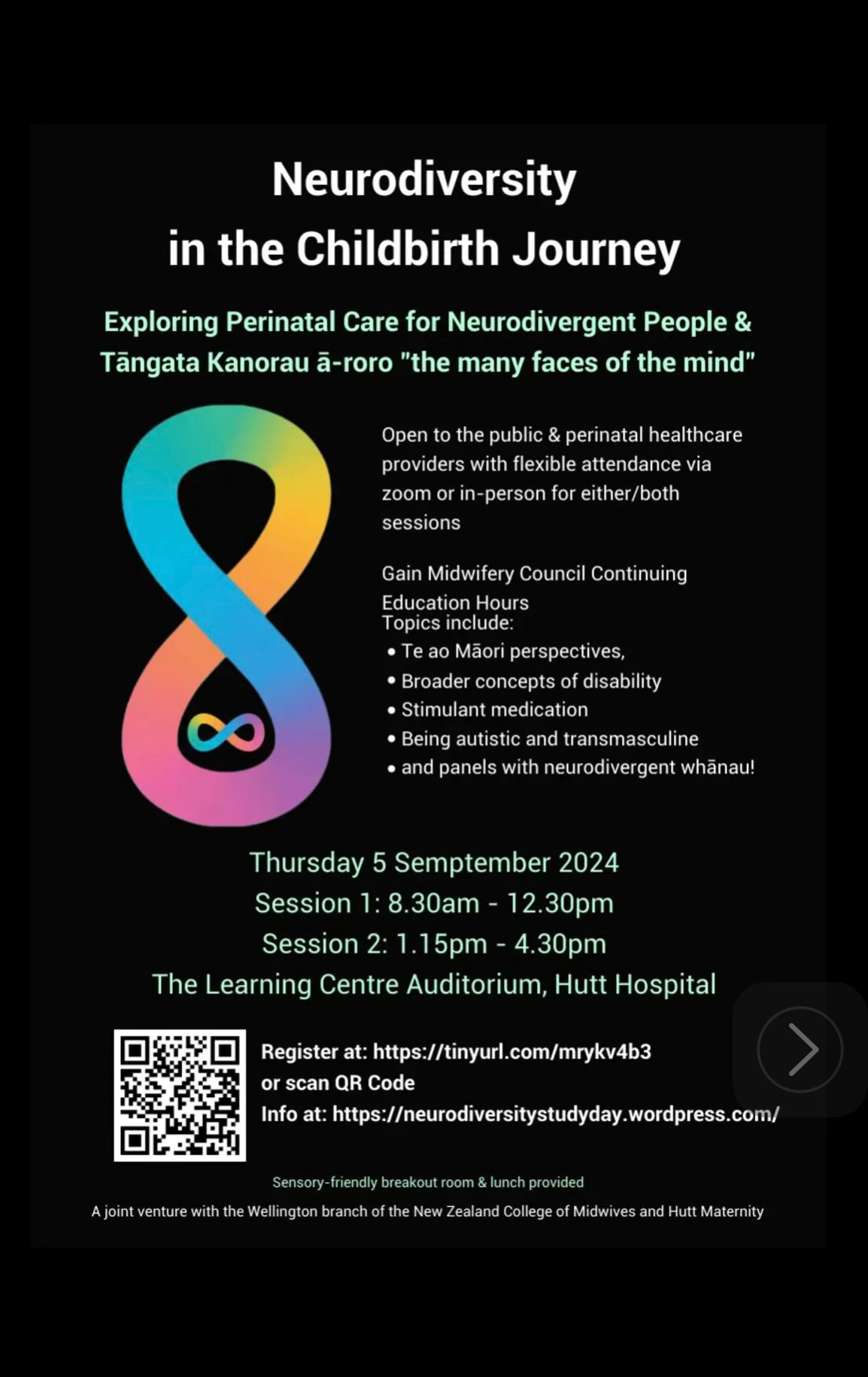
Neurodiversity in the childbirth journey
Exploring perinatal care for neurodivergent people and tāngata kanorau ā-roro
Kia ora koutou/hello everyone!
Today I was lucky enough to have participated on a kōrero/discussion panel at a study day on adjusting to the early days of neurodivergent parenting, here in Wellington, Aotearoa New Zealand.
Thanks to the organisers - neurodivergent midwives, academics and podcasters - and Bronwyn Rideout for inviting me onto the afternoon panel, and for hosting such a great study day! You can listen to The Neurobirth Podcast here, which I would highly recommend.
With my auti peri brain fog being at an all time low (or is it a high? Anyway, it’s dreadful), I had to labour (excuse the pun) over the discussion prompts that were sent in advance. I could not rely on my working memory to hold the question and my response in my head, and speak the words in any semblance of sense. So, in my head, it morphed into a scripted Q&A. I had no capacity to ad lib, at least not without going well off topic and launching straight into amateur comedian Sam territory. Oh how I have missed being on stage with a mic in hand, and I didn’t even have to make anyone laugh! 🎤
Although I have an awkward tendency of trying to make people laugh regardless, even if it’s inappropriate, which it kind if is, in the context of our collective past trauma 🙈
Anyway, I had so much to say once I got writing on the topic, that I wanted to share it with you!
I would love to know if any of this is relatable to you? Or if you have had a different experience of neurodivergent pregnancy and early postpartum weeks?
It was fascinating reflecting on my postpartum weeks again through a neurodivergent lens, and remembering the hormonal nightmare that characterised those early days of motherhood for me. I feel saddened for my pre-diagnosed self, who couldn’t understand why my experiences were so different and challenging from everyone else around me.
My sons are 12 and 9 now, and we were all diagnosed AuDHD just a few short years ago.
I certainly have been the emotional victim to my hormones during the life transitions of puberty, menarche, PMDD diagnosed retrospectively in peri, as well as autistic perimenopause itself. Remember, just because these hormonal transitions are “natural and normal”, it doesn’t make them easy for anyone, particularly those diagnosed/pre-diagnosed autistic. A good predictor of an extreme perimenopause is having extreme experiences of menstrual cycle/hormonal transitions throughout our lives.
True to form, I was hot flushing all through the discussion. Hopefully my chemical menopause will kick in properly soon, and I will cool down before Summer arrives down here in Aotearoa.
And without further ado, here are my prepared responses to the discussion prompts today…
What does being neurodivergent mean to you?
My presentation of neurodivergence is one of internal conflict and opposition, which causes struggles at all times. This is especially so during major hormonal shifts, including postnatally. Being autistic, I require familiarity within my environment and the company I keep, whereas also being ADHD, I get bored with routine and can be very impulsive. I have a natural inclination towards anxiety and panic, which is hormonally exacerbated, which also causes depression and mental health challenges.
My neurodivergence makes me thoroughly research everything, and to strive for perfection. This was especially so before I identified as autistic and ADHD. I am now more forgiving and compassionate with myself. Upon reflection. It may have been part of masking to find out how I “should” be behaving.
I am hypersensitive to sensory stimulation, my environment, judgement from others, and I do not like to take advice. As a PDA autistic, I have a pervasive drive for autonomy. I am a deep empath and take on other people’s emotions unintentionally. This can be highly distressing.
Thanks to my neurodivergence, I am very creative and can find solutions to problems that may allude others. This makes me tenacious and determined, for example when breastfeeding my babies to full term, despite ongoing disapprovement from others and going against social norms.
I often back up my choices with research and data, which non-autistics and laypeople find endlessly frustrating.
How did your neurodivergence influence your postnatal journey?
My neurodivergence characterised my pregnancies and postnatal times, although I was not yet diagnosed. My extreme hormonal levels caused me to feel out of control, vulnerable, manic yet depressed, very tearful, hopeless and I could not assimilate my bodily changes into my sense of self. It was very upsetting not recognising myself in the mirror.
Neurodivergence ensured I was well read on attachment parenting as my chosen method of bringing my baby into the world. I was so determined to do things my way, and insisting it was the best way for us that it caused friction and resentment. “Us” meaning the baby and I. I think I felt so out of control in my own body and mind, that I pulled back control in whatever way possible. I exclusively breastfed both my sons, as the “breast is best” rhetoric made me feel a failure for undiagnosed tongue ties in both sons.
I struggled with never again being able to be alone, to be still, at peace, emotionally regulated. I was conversely also overjoyed and overwhelmed by early motherhood, in awe of my babies and completely unable to rest and recover. I was being relied upon entirely by them, and my decisions counted, I took this responsibility very seriously. I was not much fun for anyone else any more!
I rejected all interference and was often unable to speak up for myself, even though I always believed that my choices were the right ones. I was unable to verbally justify them, and this caused a great deal of conflict. Sensory and emotional overwhelm makes me unable to speak.
I saw our first son’s birth weight loss as a personal failing, and had meltdowns in the hospital when this unnecessarily became medically managed in the UK hospital where I birthed him. I experienced extreme trauma at this time and, in hindsight, they should have sought psychiatric assessment, but this was never mentioned. An earlier autism diagnosis at that time would have eased the early years of parenting, particularly when I became a mother of two in complete overwhelm, with two undiagnosed neurodivergent toddlers. When I had needed the most support, there was none. This has impacted on my mental health and my traumatic and early perimenopause, building on negative thought patterns and internal struggles.
I was always very conscious of getting things wrong, so I was determined to stand my ground. This may be externally apathologized as “rigidity”, and less formally as “stubbornness”. Now I know that it was a trauma response from undiagnosed neurodivergence.
The signs of depression in autism differ from neurotypical people. Probably even more so postnatally.
During your postnatal journey did you experience any specific sensory needs, differences or changes?
Yes, lots!
Postnatal bleeding was horrendous and a major offence on my senses - the smell, the feeling of oozing and passing clots, the washing of raw and sutured skin was too much to bear, all while caring for a new baby. It lasted far longer than I could have anticipated and I didn’t now how to cope with it at all?
Due to undiagnosed tongue tie with my first son, and a TT snip on day five with my second, we had an suboptimal latch. My milk production was low so I always had my babies on the breast when they were tiny. Oxytocin was my constant goal and reward. I wore them on me using wraps and slings, keeping and needing them close, whilst dreaming of personal space. I was constantly touched out. The increased heat, the baby noises, the dribble all down me, was all a lot to process. As I didn’t know I was autistic, I didn’t even know that these were issues of hypersensitivity at the time. All my energy was spent co-regulating my babies, but I was deeply dysregulated.
It would have been beneficial to know that I didn’t have to accept visitors, and that I could have asked for help when I did let them in. I hated when they wore strong perfume, held my baby, then gave them back stinking of perfume. That always upset me for days afterwards, as I have sensory processing differences and am deeply affected by scent.
The sound of babies crying is deeply upsetting to me as an empath, and I have no tolerance for it whatsoever. To solve this with my own babies, I nursed them on demand at all hours and always fed them to sleep, I coslept (I still cosleep with my nine year old or he feels unsafe) with them and I wore them on my body most of the day. This was not great for my back, but it was necessary at the time. As they were also undiagnosed autistic and had separation anxiety, this was beneficial to forming our attachment. Autistic attachments may look different to non-autistics, and need validating and supporting.
Constant handwashing, nappy changing and chores made my hands chapped and painful, but I had to keep using them regardless!
Basic self-care and personal hygiene tasks were much harder to fulfil with a newborn. Not completing my everyday tasks in order is distressing to me, and this exacerbated my OCD tendencies. Constant hormonal fluctuations impact my capacity, functioning and moods, causing extreme and unavoidable sensory overload. What little capacity I had at any given time was dedicated to the baby’s care, leaving nothing for me. ADHD makes it difficult for me to prioritise tasks in order of importance, rather than by interest, which was a challenge as I could no longer do anything I liked. My self-regulation tasks such as attending live gigs and stand up comedy shows, and even baking and crafting could no longer be completed, so the sensory demands placed on me far outstripped my capacity to cope with them. There was no chance of gaining internal equilibrium, and this builds up over days, weeks, months and years of neurodivergent parenting.
During your postnatal journey did you experience any specific communication needs, differences or changes?
Yes again, lots! Neurodivergent people will often have lifelong difficulty with sleep, this impacts on our capacity to communicate. Sleep deprivation with a newborn will increase this, and some people will be unable to communicate with healthcare practitioners, especially when bonding and communicating with baby takes their priority. I was extremely responsive to my newborn baby’s cues and communication, but had nothing left and no tolerance for adults at that time. It was difficult to switch between these demands on my attention, especially as adults didn’t comprehend that I had had no sleep whilst trying to to establish exclusive breastfeeding. My communication with the baby was heightened, and I was hyper vigilant to their needs. I couldn’t understand why any adults would want anything from me when I was already so busy, so this caused conflict.
In the UK where I birthed my babies, NCT groups are part of the professional middle classes’ coping and education strategies. They purport mainstream parenting ideals and begin antenatally. Often groups then continue to meet informally with new babies and share birth stories, build friendships and encourage each others’ mainstream parenting methods. I was the odd one out, but had no alternative connections. I later found local baby wearing groups and found some new like-minded friends.
I was hysterical a lot of the time and, upon reflection, that was due to previous medical trauma around pregnancy losses. Bleeding is extremely triggering to me due to those losses, but this was not something I had the capacity to process, understand or express verbally at the time. I reacted to difficult situations with meltdowns and shutdowns, but they were perceived as being overly dramatic and moody or over sensitive, because I wasn’t diagnosed autistic at that point. Anything that was later seen in context as a trait of neurodivergence would have been misjudged as a character flaw or moral failing on my part. Therefore masking and camouflaging my differences was a crucial survival technique, but placed extra strain on my capacity.
It was difficult because my attachment style of parenting required me to defend my choices at all times, since others didn’t see them as important or valid, and wanted me to just be like everyone else with my baby. As a trauma response to a lifetime of judgment and shame, I tended to just weep under pressure, completely unable to express myself.
Autistics need a lot of time and headspace to process communication and information, and this just isn’t possible with a totally dependent newborn in your arms at all times. Therefore I out all my energy into the babies to the detriment of all my other relationships. I lost a lot of friends at this time of life, but have since had the opportunity to form other friendships with like minded people with whom I can be completely myself.
Booking and attending appointments is a major challenge for neurodivergent people, so making them for my newborn and requiring me to bring along paperwork etc. was a big strain on my executive functioning skills. When bleeding, in pain, having had a traumatic hospital readmission for birth weight loss and struggling with breastfeeding, attending regular weigh ins was cruel and always triggered a meltdown from me at the baby clinic. I did not have the capacity to articulate any of it, but it would have been helpful to receive an adult mental health referral from the health practitioners who would have witnessed my extreme distress. I was masking heavily and would have convinced them I was “fine”, but I needed judgment-free support and compassion.
I had difficulty speaking up for myself due to feeling overwhelmed, scared and anxious at all times. These are lifelong tendencies for me, and I can mask them exceptionally well, but they increased postpartum. I had to spend a lot of energy trying to suppress intrusive thoughts and OCD behaviours.
I eventually went to the GP with my husband about my mental health struggles, and received a postnatal depression diagnosis. I was referred to a counsellor which was helpful, and she advised me that it was postnatal anxiety, rather than depression. I was also referred to group CBT sessions with other first time new Mums run by two NHS social workers. That was helpful too, but I believe a basic screening for all new mothers experiencing postnatal mental health issues, especially with previous episodes during hormonal transitions (puberty, pregnancy, postpartum) should be assessed for autism. It would prevent a great deal of trauma, misdiagnoses, self-harm and suicidality later in life, especially as three times more autistic women die from suicide than non-autistics in midlife. These deaths are preventable, if only we understood ourselves better, and if the medical system could better communicate with autistic women during hormonal life transitions.
Communication tips for supporting neurodivergent people:
Avoid small talk
Be literal, clear and concise
Use medical terms and explain them
Presume competence, not getting a spoken response doesn’t mean we don’t understand
Allow extra time for processing information you give us, particularly if it’s a shock or unexpected. Just because we don’t look or act worried, doesn’t mean we aren’t feeling that way
Tell us in advance of any house visits, don’t just drop in unexpectedly
Text us rather than call, if possible
Let us know any next steps we should anticipate, and provide them in writing if possible
Provide visual supports if we are going to be bombarded with information
Be aware that we can experience anxiety in social situations, and with unexpected changes
What did your healthcare providers do well to accomodate your needs/preferences?
With my second baby, I chose a home birth. I had a private doula, two midwives and a student midwife. I was familiar with them all due to consistency and continuity of staffing, which had not been the case with my hospital birth. Subsequent postpartum appointments were with the home birth team, unlike the inconsistent healthcare practitioners visiting after the hospital birth. Continuity of staffing is vital for neurodivergent postpartum parents, as we build a relationship with them over pregnancy, that carries over into postpartum life. We are better able to communicate with them, and them with us since we are able to get used to each other and feel safe and comfortable.
They understood that I was exhausted and were always compassionate.
They never passed judgment on my appearance nor the state of my house, unlike some family members.
When my first baby was readmitted to hospital on day 5 following a drop in birth weight, they let my husband stay overnight with us, as I was having meltdowns and was not functioning or coping
With the second baby, they explicitly trusted my judgement and let me lead breastfeeding, but I had to initiate La Leche League home visits, and lactation consultant visits that I had to attend alone out of town with my newborn five days postpartum.
What could the healthcare providers have done better to accomodate your needs/preferences?
With the first baby, they did not check for tongue tie despite birth weight loss, so I was left wrongly assuming the fault was with my milk supply, our inadedquate latch, positioning, etc. Basically I was left thinking that I was a terrible mother and incapable of caring for my baby, hence the meltdowns. I speak with a lisp, they should have checked for a tongue tie at birth and snipped it. My rumination and anxiety needed soothing by proper medical examination, not overriding my decision to exclusively breastfeed by prescribing bottled formula. Telling me I didn’t have enough milk for my large newborn so I shouldn’t feel bad for supplementing them made them feel better, but it made me feel worse. Many autistic mothers will choose to breastfeed to natural term - my sons were almost five when we stopped nursing. Our choices may not be everyone’s preference, but we need bodily autonomy to make our choices or we can feel emotionally and psychologically unsafe. Please trust our decisions and support us.
Referred me to public adult mental health services
Booked home visits, rather than dropping in, so there were no surprises or changes to plans
Providing reading material and visual supports for information
Giving me extra time to process responses verbally
Letting me know that baby weigh ins were not essential and that I had the right to decline them, which would have spared me traumatic flashbacks and public meltdowns
A postnatal care plan, written in detail like the birth plan, would be an excellent way of supporting and signposting new neurodivergent parents in the childbearing journey
Presenting any information in an easy read format with visuals, essential details and social stories would support us through this transition. Externalising our memory reduces the mental load on our executive functioning capacity
Providing photos of the healthcare team so we know who to expect will be helpful and support us with face recognition differences
Offering appointments via Zoom or using email/text to communicate can be easier for us than phone calls and home visits, where possible




Congratulations!
Thank you for sharing your experiences - there is so much insight here, and a lot that I relate to. Having that insight that I was neurodivergent would have been a massive help for me in the years after I had my kids.