10 Tips for Managing Autistic Hormonal Depression
Did you know postnatal depression (PND) and premenstrual dysphoria disorder (PMDD) are predictors of menopausal depression? Forewarned is forearmed.
Hi Team Auti Peri, how are you? 💕
Since stopping my mood stabilisers (they are supposedly sedating, but caused insomnia for me 🤷♀️) and having my Mirena IUD removed a couple of weeks ago, my ragey mood seems to have stabilised and picked up finally. I am hoping this lasts a while, but I know how unpredictable these things are in autistic perimenopause so let’s just wait and see what is in store for me next…
I am working on my book proposal about autistic perimenopause, and my head is stuffed with Auti Peri-ness…
I hope you are doing okay?
Apologies - I have been in your email inbox a few times this week already and am feeling worried about taking up too much space - physically and digitally!
This is a long one and won’t all fit in your email inbox, so please open it on the Substack website or in app to read the entire thing.
💕
Thanks so much to Autistic Ang, Tamsin Chennell and Allegra Chapman for participating in The Auti Peri Q&A Series!
In case you haven’t had a chance to read them yet, here are all The Auti Peri Q&As published so far. I am delighted to say there are more to come!
I would love to make this an ongoing feature and would love to share your story of autistic perimenopause! Please reply to this email if you would like to feature in the series. If you are reading this in the Substack app or website, please feel free to DM me and I can send the questions over to you.
The more stories we can share and read, the better informed our community will be on the varied experiences of autistic perimenopause!
💕
My first Substack live!
A couple of days ago, ND creativity coach and author Allegra Chapman and I spontaneously recorded a live video together which was fun! Our goal was 10 minutes, but thanks to ADHD we got to 19 minutes when I realised I was late for an appointment.
You can just listen to the audio podcast style if that is a more accessible format for you. 🎧
The REPLAY:
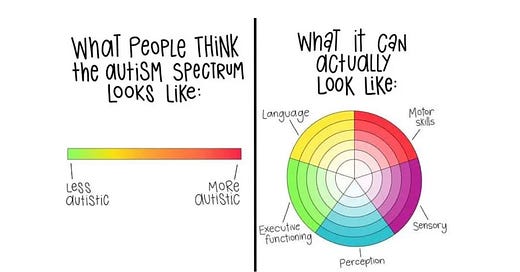
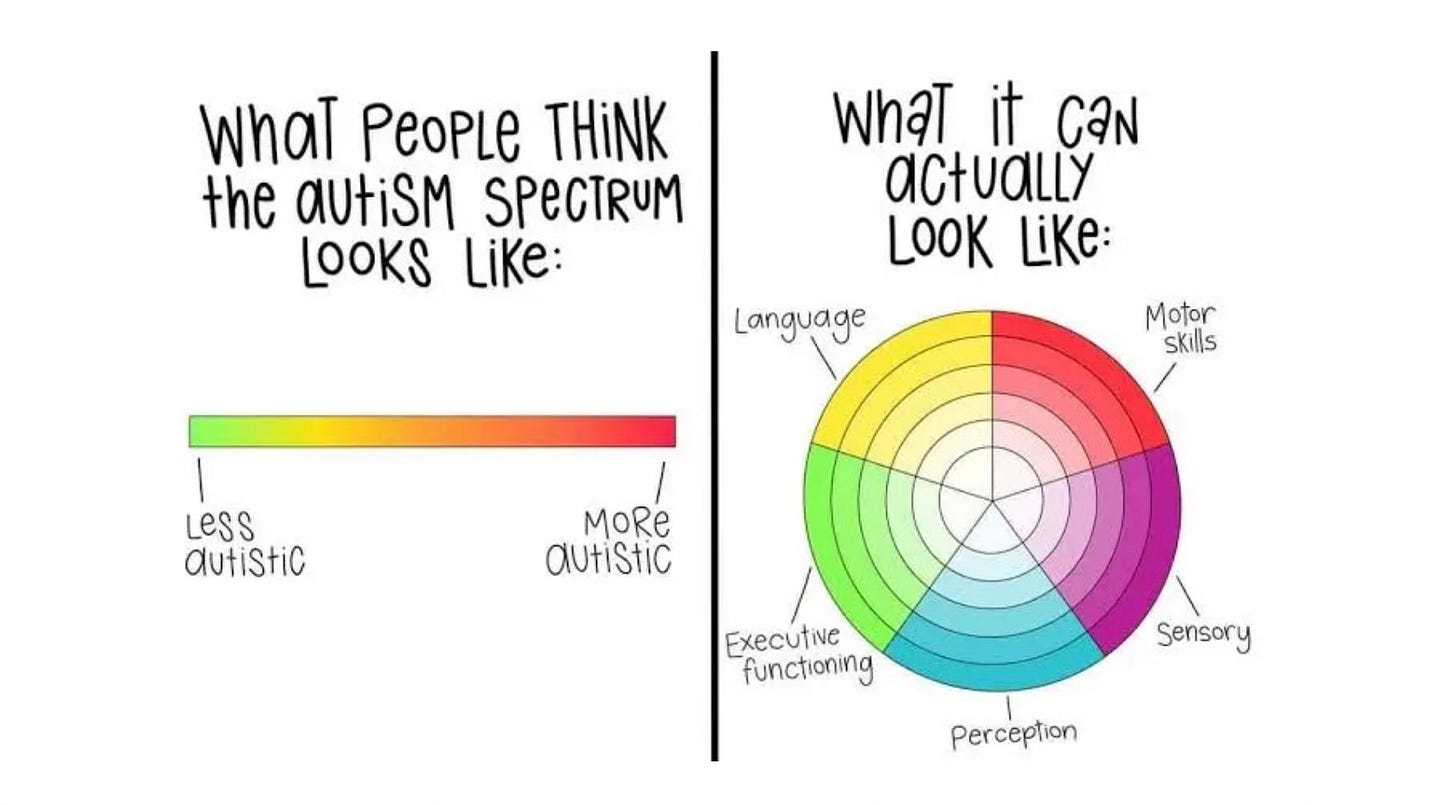
Just for the record, where the closed captions say “secular”, I in fact had said “circular” and this is what I was referring to:
10 Tips for Managing Your Autistic Hormonal Depression
Did you know postnatal depression (PND) and premenstrual dysphoria disorder (PMDD) are predictors of menopausal depression?
Forewarned is forearmed.
Westernised society values ever growing progress as a key marker of success, which is why disabled and neurodivergent people may find themselves being pushed out to the margins throughout our lifespan.
A known marker of childhood autism is asynchronous development and fluctuating capacity, meaning that one day an autistic child can stay regulated in a familiar environment, and the next day in the same place they might be distressed and having meltdowns. Asking them why they can’t cope today when yesterday they could is pointless, as is telling them to “pull themselves together and get a grip” (ask me how I know).
Autism is a lifelong dynamic disability, characterised by fluctuating capacity and periods of functioning. When an autistic adult is outwardly appearing to “cope” in the same environment day in, day out, we may not be internally feeling the same every day. As a highly sensitive population, we may be reacting to and overloaded by environmental factors such as background noise, over scheduling our calendar, even the weather. Internally, we may also be exquisitely sensitive to hormonal fluctuations, hot flushes; sitting down may be painful if we have vaginal atrophy and UTIs. Autistics have a reputation for not empathising with others and picking up on social cues but, since autism is a spectrum condition, many of us are painfully aware of our social environments, and see the eye rolls, and hear the snide remarks made about us behind closed doors. Yes, our auditory processing can be so precise that we can hear everything that is said about us, and it hurts more than anyone can imagine.
Despite all of this, we want to be accepted for the humans we are, so we internalise the rejection and the pain. Somehow, despite the odds, we suppress a meltdown - which may be an outpouring of repressed grief as much as a response to that noisy freight train that just went by the building. What I am clumsily trying to say is that we are often masking and socially camouflaging in order to look like we are coping, because we have learnt the hard way that looking distressed and having meltdowns makes other people reject us. Do you have any idea how exhausting it is to feel ongoing deep pain and dejection, whilst having to force on a smile and pretend you are fine?
Well, at some point that all becomes too much to bear. By midlife - if not before - the weight of the mask can become too great, our face starts revealing what we didn’t want people to know, and we may have meltdowns or shutdowns of increased frequency, intensity and duration. In public, whereas before we saved them up for home… The Rage can spike, and you may release decades of pent up fury with no warning whatsoever. This is terrifying (ask me how I know!)
But this can be part of the autistic perimenopausal transition, and if we know why it is happening - and understand the physiological mechanisms i.e. that it’s not our fault - it can be liberating and validating to finally express ourselves in all our autistic glory. When and where we feel safe in doing so, hopefully.
During autistic perimenopause, hormonal fluctuations cause temporary regressions and loss of self-care skills. Those of us who have been fortunate enough to have survived postnatal depression (PND) as a one off, and/or recurrent episodes of premenstrual dysphoric disorder (PMDD) are more likely to experience menopausal depression, as we are highly sensitive to changing hormone levels.
Why does knowing this matter?
Because we know first hand how scary those depressive bouts have been. We have had to precariously live our lives balancing the scales between masking our moods for the benefit of others, and setting accommodations for ourselves by avoiding certain people and situations. Camouflaging our deep sense of impending doom. Trying to suppress and fight off thoughts of self-harm and suicide. Telling our face what to do in the company of others, whilst inwardly fighting off intrusive thoughts of harming coming to the people we are trying to protect.
This matters because PND and PMDD are both relatively well known mental health conditions. Albeit difficult to admit to and recognise in ourselves, when we push so much energy into hiding them. PND is a condition affecting many new parents, and PMDD is regular and predictable. A predictable mental health condition can be accommodated and better supported when it is regular enough to be monitored and medically managed.
But perimenopause, by its very nature, is a life phase characterised by unpredictability and constant flux. In autistic perimenopause, we can not anticipate hormonal peaks and troughs. This is the danger. Those of us who are highly sensitive to fluctuating hormone levels needed the former consistency of menstrual cycles to plan our “good weeks” when we flourish and thrive, and our “awful” weeks which are a total write off. The weeks in between are “meh”, but somehow we get by.
Our mood changes can be so rapid and unexpected that we are unable to anticipate them in advance. But there is no need to feel hopeless nor helpless. We can protect ourselves by creating a safety plan to buffer ourselves when hormonal fluctuations occur, and stay safe when suicidal episodes occur.
In no particular order (because what are we, if not asynchronous and dynamic?), here are my 10 tips to managing hormonal depression in autistic and neurodivergent perimenopause.
1. Read up on menopause and perimenopause.
General information will have to suffice for now until there is more specific support and information available about the autistic experience of menopause. Social media is great. It can be informative and validating, but please only take medical advice from medical professionals and reputable sources. If someone is trying to make money from you (supplements, diet plans etc.), they are not impartial. Be cautious with your care and your cash.
There is *just* enough empirical research and information out there for us to feel our way through autistic perimenopause, but we are still currently in a data void of academic research for our neurotype, so we have to use the general meno advice and medical information available to us. Some of this may not feel appropriate due to our neurology, but some may apply. You can take or leave what you find out, but please do educate and inform yourself. Knowledge is empowering.
For super geeks (hello friend!) like me, you might like to deep dive into the British Menopause Society (BMS) Tools for Clinicians. Once that has whet your appetite you might like to continue your research in the Australasian Menopause Society website, with sections for patients and professionals.
🤓 I have compiled everything in my Resource Roundup post that I have come across so far about autistic perimenopause online, and it is in the navigation bar of The Autistic Perimenopause: A Temporary Regression homepage.
Resource Roundup: Everything about Autistic Perimenopause in one place
Autistic perimenopause is becoming increasingly well known, so let’s keep the momentum going.
Yes, you may well end up knowing far more about peri and menopause than your doctor or healthcare professionals, but I think that can only be a good thing! Hopefully they will all catch up soon…
2. Track/journal your symptoms.
I am so sorry! I know this is hard for many of us with executive functioning challenges, which are so often exacerbated periodically during autistic perimenopause. Particularly for anyone like me who is a PDAuDHDer (pervasive drive for autonomy autistic ADHDer defined by resolutely characteristic demand avoidance), who not only does NOT want to be told what to do, but will refuse to engage should you try and tell me.
I have some resources that you might be interested in looking over below, but absolutely no pressure.
Personally, I have been in many medical appointments about my auti peri and been flummoxed by totally predictable questions such as, “What date was the first day of your last period?”… 🧐 🤷♀️
Tracking isn’t essential, but let’s just say the more insight and data you have to share with your healthcare team about your individual physical and psychiatric symptoms, the quicker they can titrate your medications/HRT, therapies and treatments.
Tracking symptoms helps you to eventually have buffered hormones, controlled/predictable bleeding, stability of mood, and supports in place to hold you through the toughest of times, which is absolutely the goal here. Well, it’s my goal, but may not be yours.
Journalling: not necessarily as a means in and of itself, because surely nobody can journal themselves out of a sense of sudden and utter desolation… But alongside keeping a note of your symptomatic ups and downs it is beneficial, and there are tools to help you:
printable menopause symptom trackers,
There is also the beautiful option of The Perimenopause Journal: Unlock Your Power, Own Your Wellbeing, Find Your Path, by Kate Codrington.
What is ironically important to remember here is that you don’t have to remember anything. If you log your symptoms fairly regularly into any type of system, it will support you where lagging/regressing/processing differences of intereception and working memory challenges may trip you up.
Also, seeing doctors and attending healthcare appointments can be a sensory and logistical assault on the autistic mind, body and soul, so the less cognition and recall required of you in the moment, the better you can set yourself up for a productive consultation.
Nobody knows you and your body better than you do. But, in a clinical environment within a time restricted appointment, the sensory and emotional overload may reduce your capacity for communication. It happens to the best of us. Your healthcare practitioner is bound to love the data analysis of your symptom tracker too, so self-advocate to share the joy! 🤓 📈
3. Meno-D regularly
Yes, I believe we should all by now be using “Meno-D” as a verb. And so I put it to you, “When was the last time you Meno-D-ed?” Really? Go do it now! I can’t believe we aren’t all Meno-D-ing at least once a month. More often if we are experiencing menopausal depression symptoms.
Here’s a refresher of what they are:
low energy
paranoid thinking
irritability
self-esteem
isolation
anxiety
somatic symptoms (headaches, joint and muscle pain etc.)
sleep disturbance
weight gain
decreased sexual interest
memory problems
difficulty concentration.
What do you need to get yourself regularly Meno-D-ed? This link.
It looks like this:

If you only track one thing during autistic perimenopause, please track your mood.
Mood and the Menopause by Australasian Menopause Society.
I have so much I could say about hashtag My Meno-D Life, but I need to move on…
I will share another post about it soon including an email response I received from Professor Kulkarni last year, when I emailed her an enoromous outpouring of despair about how slow the research and clinical world is on supporting people in autistic perimenopause.
4. Communicate autistically
What do I mean by this? Well in my case, I mean email very important professors of female psychiatry and academic doctors of note and tell them how worried you are about autistic people being under supported and susceptible to increased suicidality risk.
Note to self: they already know, and are doing what they can at the pace that modern non-male medicine permits, with very little funding and even less public awareness.
On a more everyday note, communicating autistically could also involve interacting without using mouth words to doctors and medical professionals (via email, text messages, online secure medical portals - more to come on this regarding Telehealth).
For some people, it may mean using Augmented Alternative Communication (AAC).
If you can and it would help you, you might like to take a chaperone/relative to appointments who can voice record or take notes on the consultation, so that you can review it at home with appropriate processing time and act on the medical advice given.
What other suggestions do you have on this? Sorry I am so busy non-stop Meno-D-ing these days that I am hyperfocused over there and ironically unable to communicate about communication.
Please share what works for you in the comments.
5. Find a doctor who understands menopause
I have covered this a lot, so please delve into my archives for more on this. Here are some of the best:
Resources and advice to support you in accessing adequate mental and physical health care and treatment in autistic perimenopause
Who can we trust to provide neuro-affirming menopausal health care and support?
Ten steps to get help and survive the worst days/weeks/months/years of autistic perimenopause
6. Use Telehealth
7. Hormonal Depression responds to hormonal therapy
Whaaaat?! I know - social media influencers have made this highly contentious, and even the medical system isn’t clear on this. Female/AFABs often see a doctor in midlife presenting with anxiety and/or depression, are sent home with an SSRI, and find that it does little to nothing to alleviate their symptoms.
That tends to be because sensitivity to hormonal fluctuations is the issue. I found out the hard way that it isn’t my hormone levels that are the problem, but the differences from day to day that affect me. Badly. So a reduction or increase would occur, but whether levels were “high” or “low” didn’t matter so much as the fact they had changed.
Sertraline is my BFF, and I won’t be parted from her. I am not saying anything against SSRIs, they are life-preserving for my midlife mental shitshow. And also so is my HRT/MHT. As in, without the combination of pharmaceuticals and hormone therapy, I would not be sitting here writing this right now.
Menopausal depression is serious and needs to be taken seriously with informed medical practitioners to help you titrate whatever treatments you need. Not whatever someone on Instagram tells us all is enabling them to live their best life.
8. Cancel plans
Whatever the thing is that will push you over the edge, don’t do it. Tell them you are beyond capacity. Actually, you don’t owe anyone an explanation. Just say no.
Unless they are employing you and you need the job? In which case, tell them that you want to, you are trying and that you need support.
Neurodiversity and menopause: what employers need to know
Menopause, neurodiversity and the law (UK)
9. Hang in there
Menopause is inevitable for all people with uteruses. Many people will sail through and not be too bothered by their symptoms. Yay for them.
If you are like me, and your reproductive system feels like it is hijacking your brain and wants you dead, please know that you are not alone.
The Autistic Perimenopause: A Temporary Regression is here for you.
Expert academic researchers are working so hard to get our plight into public awareness.
Doctors and healthcare practitioners who are knowledgeable on menopause and neurodivergence want to give you the support you deserve.
This too shall pass.
10. Have a suicide safety plan
Some days it might feel like it is all too much, and that is a totally valid feeling. But feelings aren’t facts, and they do go away.
Before things escalate, get yourself Meno-D-ing on the daily. When you feel at your worst, rate your score on the scale.
Call your doctor, call a friend, message me or join the chat. It is pretty quiet there but one of us will see your message and is bound to be awake. This community is global so we cover all timezones!
Your physical, emotional and psychological safety are absolutely paramount. Please don’t underestimate how rapidly and drastically your mood can decline in autistic perimenopause. It can change so fast that you think you are losing your mind and are a burden to others. You aren’t, and this isn’t your fault.
If you have had PND and PMDD before, you may be filled with dread already knowing how this can feel.
Reach out for help, and have an autism adapted safety plan (AASP) in place:
The resources are suggestions to help you understand and complete the safety plan for yourself, or to support another person to complete their safety plan.
Step 1 - What are my warning signs that I may start to have strong thoughts, feelings or urges to hurt myself and/or end my life? (e.g., reduced enjoyment in a strong interest, change in routine, change in patterns of sleep, eating, mood)
Step 2 - What can I do to help distract myself? (e.g., engage in a particular activity or interest, a relaxation technique, or physical activity)
Step 3 - People I can contact to ask for help: (e.g., family, friends, mentor, support worker). Remember to note down when people are, or are not, available (e.g., office hours).
Step 4 - Professionals or agencies I can contact during a crisis: (e.g., Samaritans, Mind, A & E, Psychiatric Services). Remember to note down when people are, or are not, available (e.g., opening hours).
Step 5 - What can I do to make the environment around myself safer? (e.g., throwing away things that could be used to harm yourself)
Step 6 - How can other people help support me?
How do I communicate distress? (e.g., I shut down, I have a meltdown)
What stresses me/makes me unhappy? (e.g., loud noises, being touched, change of plan, too much information)
What can help calm me/makes me happy? (e.g., a strong interest, a quiet safe place to calm down, just sitting with me, giving me my own space)
How I would like you to communicate with me? (e.g., don’t ask me to look you in the eye, speak softly, use visual supports, use plain English, keep in mind that I may take what you say literally)
Who I would like you to contact?
Step 7 – Sharing my safety plan: It can be helpful to share your safety plan. This might be with a trusted friend or family member, health care professional, or support worker. Would you like to share your safety plan? Who would you like to share it with?
Storing my safety plan: It can be helpful to think about where you will keep your safety plan so that you can easily access it if you need it (e.g., printed out, in my bag, in a ‘crisis box’, on my phone). It might also be useful to think of any prompts that could help you to remember to use your plan (e.g., having a card with the safety planning logo in it in your wallet to remind you that you have a safety plan).
Further information on AASPs is at the end of this article:
Gosh, is that the time? I am late for my latest Meno-D-ing! Are you up to date with yours?
Thanks for reading.
Take care of you,















No you're not taking up too much space digitally (for me) by appearing in inbox multiple times a week. Then again, my brain rarely differentiates between "Now" and "Not-Now" so while I understand on a theoretical basis the concept of "week", in practice it means very little so maybe I'm not the best person to ask!