Hello!
If you are new here, welcome to The Autistic Perimenopause: A Temporary Regression!
I am Sam - a late diagnosed neurodivergent woman, a tenacious midlife struggler, and an advocate for people in autistic perimenopause.
Today I am deep in the midst of neurodivergent perimenopausal misery, so let’s see if I can put words in an order that conveys anything of interest and/or that makes sense… 🤞
April is Premenstrual Dysphoric Disorder (PMDD) Awareness Month, as well as Autism Awareness Month. Yippee! 🎉
Geopolitically, the awareness drive doesn’t seem to be hitting the mark, with those in power denying us any sort of respect or rights. But let’s pop that aside for now and imagine we are receiving the support and respect we deserve for being the differently wired legends that we know we are.
💕
What is PMDD?
Premenstrual dysphoric disorder is a cyclical, hormone-based disorder that impacts approximately 1 in 20 reproductive-age women who were assigned female at birth. The condition is often underdiagnosed, misdiagnosed or dismissed entirely by medical professionals, despite patient reports of debilitating anxiety, hopelessness and a variety of physical symptoms in the two weeks before menses.
UIC Today: Suicidal thoughts, behaviors linked to hormone-sensitive brain disorder
I know, I am sorry.
As it was for me, so may it be for you: yet another co-occurring condition we can enjoy adding to the alphabet soup of diagnoses we are gaining in neurodivergent midlife.
PMDD can be another great too-late explainer of why everything has been so shit for those of us being destroyed by our menstrual cycles for decades. Yay. But contextualising past (and, in my case, current) hell is a winner, right?
So, yes, PMDD is an actual “mental health disorder” and validates why many of us have felt beyond awful on a cyclical basis.
Yet with no perception of time and as a lifelong time agnostic (thanks, ADHD!), it is unfortunate that tracking symptoms and noticing patterns over time is not a strength of mine.
Whilst I can think back to the overflowing catalogue of times when former friends and ex partners have told me I am a “crazy bitch”, I wouldn’t pick up on that being, for example, the third week of every four week cycle.
PMDD is not a hormonal imbalance. The hormone levels are not the issue, rather those of us with PMDD are neurobiologically sensitive to the fluctuations of oestrogen and progesterone levels through a normal and natural menstrual cycle.
NB: I am so exhausted by PMDD and all the other midlife BS right now that I am not coping with, that I am struggling to figure out when to use the words “period”, “cycle” and “episode” in the correct context. And all this whilst my teen is sitting beside me as I write telling me about Fortnite…
Here is a very short podcast episode from The International Association for Premenstrual Disorders and provides a succinct explanation of PMDD:
In order for me not to provide you with the wrong information, let’s hand this over to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
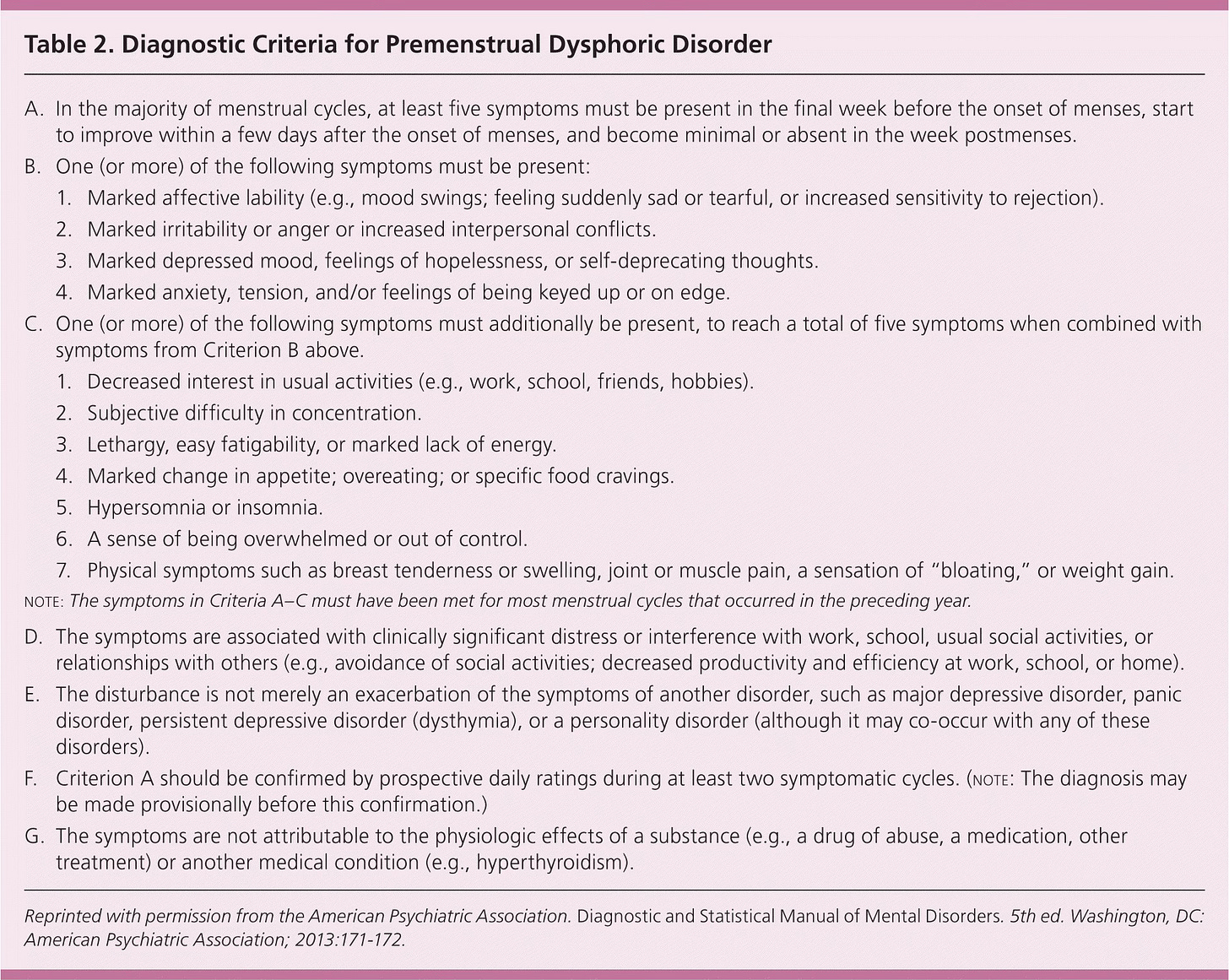
I don’t know about you, but I cannot process that text right now. Therefore, full disclosure, I have asked ChatGPT to summarise this for an autistic audience in an easy-read style:
⬇️
✅ To have PMDD, these things must happen:
🌸 What is Premenstrual Dysphoric Disorder (PMDD)?
PMDD is a serious health condition that affects some people before their period (menstrual cycle). It causes strong feelings and body changes.
✅ To have PMDD, these things must happen:
1. Timing of Symptoms
You must have at least 5 symptoms in the week before your period starts.
The symptoms:
Start before your period,
Get better a few days after your period starts,
Are mostly gone in the week after your period ends.
2. At Least 1 Strong Feeling Symptom (Pick from this list):
You must have one or more of these:
Mood swings (feeling very happy then very sad quickly)
Feeling angry or annoyed easily
Feeling very sad or hopeless
Feeling nervous, worried, or on edge
3. Other Symptoms (To make a total of 5 symptoms)
You also need more symptoms from this list:
Not enjoying things you usually like (e.g. friends, hobbies)
Trouble focusing or thinking
Feeling very tired or no energy
Eating a lot, or craving certain foods
Sleeping too much or not enough
Feeling overwhelmed or out of control
Body problems like:
Breast pain or swelling
Muscle or joint pain
Feeling bloated
Gaining weight
4. How it Affects Your Life
The symptoms make it hard to do normal things like:
Going to school or work
Being with friends or family
5. Other Health Conditions
PMDD symptoms should not just be part of another condition (like depression or anxiety), but PMDD can happen at the same time as other conditions.
6. Keeping Track
Doctors should look at your symptoms for at least 2 periods in a row to be sure.
7. Not Caused by Something Else
The symptoms are not caused by:
Drugs or alcohol
Medication
Another illness (like a thyroid problem)
(Sam) Then I asked ChatGPT for a diagram to support the visual processors amongst us 🙋♀️
⬇️
⬇️
Sam to ChatGPT:
⬇️
(Sam) ChatGPT could not fulfil this request, so let’s not get too worried about AI coming over here and taking our jobs and our women just yet.
*** END OF CHATGPT AND AI USE IN THIS POST *** (apart from the transcript from my audio voiceover that Substack tech will hopefully write up for me later)
💕
Why do I need to know if I have PMDD?
Increased risk of suicidality is associated with PMDD, and that is why I want you to know about it. It is also more prevalent in the neurodivergent population, which I doubt will shock you.
It is tricky, as it can take decades before we realise this chronic mental health condition affects us. I was diagnosed with it retrospectively after unwittingly undergoing the third line treatment for this little known debilitating mental health condition.
Before I knew I had PMDD, I heavily masked my cyclical breakdowns, took a lot of time off work (I was a teacher in my 20s), binge ate chocolate, then manically exercised to compensate for it. I lost close friendships, stormed out of the house with no plan where to go and not knowing why I had put myself in that vulnerable position. I drove dangerously, and leaned into impulsivity. I raged and had intense meltdowns, smashing things a la Fern Brady in her autistic memoir, ‘Strong Female Character’.
Whilst it is helpful to know now that I was a PMDD sufferer, I would have found greater benefit in that diagnosis decades ago. I could have planned my life accordingly. I masked to an exhausting extent, and made up for my self-destructive PMDD one-week-in-four episodes by pushing myself beyond my limits my three “good” weeks per menstrual cycle.
Putting all my energy into hiding and excusing this “mental disorder” each month left me exhausted and susceptible to cyclical undiagnosed autistic burnout. So now I know that understanding myself sets me up to be more aware of potential challenges, and kinder to myself when they are genuinely insurmountable.
People diagnosed with PMDD these days are able to request reasonable accommodations at school, at home and at work.
In the laughably entitled podcast The Happy Menopause, interviewee and PMDD survivor, lecturer and researcher, Dr. Lynsay Matthews, states that PMDD sufferers may describe their episodes as:
spiralling
unravelling
out of control.
And they may identify these patterns in line with the luteal phase (post-ovulation to your bleed, average days 14-28 of the menstrual cycle):
cyclical relationship crises (splitting up with your partner every month, losing friendships etc.)
cyclical addiction crises (patterns of alcohol or drug misuse, associated driving under the influence offences etc.)
cyclical psychosis crises (I don’t have examples of this but I am wondering about the misdiagnoses of Bipolar Disorder and/or Borderline Personality Disorder that so many menstruating autistics and ADHDers receive..?)
💕
Australia-based UK-trained GP with an interest in women’s hormonal health, who was interviewed on the Sexy Ageing podcast, Dr. Ceri Cashell, says:
“Life’s short. You don’t know what’s around the corner, so to lose half or a quarter of your life due to these (PMDD) symptoms is horrific.”
How do I know if I have PMDD?
IAPMD provides an online self-screening tool that is not intended to be diagnostic, but may support you in knowing whether or not to pursue an assessment. The purpose of the self-screening tool is to help you identify whether you may have PMDD or Premenstrual Exacerbation (PME).
PME, is a condition that is a worsening of symptoms of another disorder, such as generalised anxiety or major depressive disorder. It is a different condition to PMDD, but the two can be difficult to distinguish between.
What a mindfuck.
If you, like me, have used the oral contraceptive pill over the years, your PMDD may have been masked treated by this during that time. That can make it harder for us to know in hindsight that we have been struggling with this condition. Therefore, symptom tracking is required for an assessment and diagnosis.
HOW IS PMDD DIAGNOSED?
Premenstrual Dysphoric Disorder cannot currently be detected or diagnosed via a blood or saliva test. However, a blood test can rule out other conditions which would need to be managed differently to PMDD. The only way to definitively diagnose PMDD is to track the severity of your symptoms over two or more menstrual cycles.
Download the IAPMD premenstrual tracking guide to identify a possible link between any symptoms you have been experiencing and your ovulation cycle.
The trackable symptoms:
Felt depressed, sad, “down,”, or “blue” or felt hopeless; or felt worthless or guilty
Felt anxious, tense, “keyed up” or “on edge”
Had mood swings (i.e., suddenly feeling sad or tearful) or was sensitive to rejection or feelings were easily hurt
Felt angry, or irritable
Had less interest in usual activities (work, school, friends, hobbies)
Had difficulty concentrating
Felt lethargic, tired, or fatigued; or had lack of energy
Had increased appetite or overate; or had cravings for specific foods
Slept more, took naps, found it hard to get up when intended; or had trouble getting to sleep or staying asleep
Felt overwhelmed or unable to cope or felt out of control
Had breast tenderness, breast swelling, bloated sensation, weight gain, headache, joint or muscle pain, or other physical symptoms
At work, school, home, or in daily routine, at least one of the problems noted above caused reduction of production of efficiency
At least one of the problems noted above caused avoidance of or less participation in hobbies or social activities
At least one of the problems noted above interfered with relationships with others
Source: IAPMD website
💕
PMDD and Neurodivergence
When I look at the lists of symptoms above I can see how they have characterised and dominated extensive periods phases of my life so far.
It is hard to unpick those symptoms when they can be an unfortunate way that our co-occurring autism, ADHD, anxiety and/or depression present in our lives. But I do recall that in an earlier stage of my perimenopause, I was having multiple bad weeks on the trot, would hold out for my unpredictable period that would arrive within two or six weeks, and rejoice in that one week of bliss where my mind and body felt rejuvenated.
Waiting for my period was torturous, the menstrual cramps and back pain were hideous, and the unpredictability was just cruel.
Eventually my periods morphed into one long bleed that lasted months with no reprieve, and my sensory overload was unbearable. My suicidal ideation ramped up, and I was given a Mirena coil to stop the bleeding.
The cessation of my bleed was an enormous relief on my depleted energy levels and my overwrought nervous system, but within a short time it became clear that I was not tolerating the constant low level progesterone release of the Mirena. Anecdotal evidence suggests that there may be a subgroup of PMDD sufferers who are progesterone sensitive, but of course the research evidence is lagging on this topic.
As highly sensitive individuals, we must tread our treatment paths tentatively and reflexively. Our doctors may be highly skilled (or sometimes not), but our feedback is vital in our own healthcare.
Interoceptive differences in our bodies and minds complicates this all further, in that we may feel highly sensitised or desensitised to the effects of our hormones, hormone therapy and other treatment options.
It is essential that we are aware and educated on this because suicidality is rife in our community. We can just reach a point where it all gets too much, and we don’t feel we can take anymore. I know what that feels like.
But I try to remind myself that, as much as I love statistics, I don’t want to become one. Perhaps that is due to my demand avoidant profile..? I often think that is the case, and it makes me more determined and impassioned to share what I can with you, for both our benefit.
Recently I recorded this video to walk you through the straightforward yet emotive process of writing an autism adapted suicide safety plan:
Whilst researching this topic for you, I came across Jes Fleming on Instagram who shares information on PMDD and mood.
In pursuit of balance, you might like to check out her resources as she has a naturopathic slant with the perspective of healing from rather than dealing with PMDD.
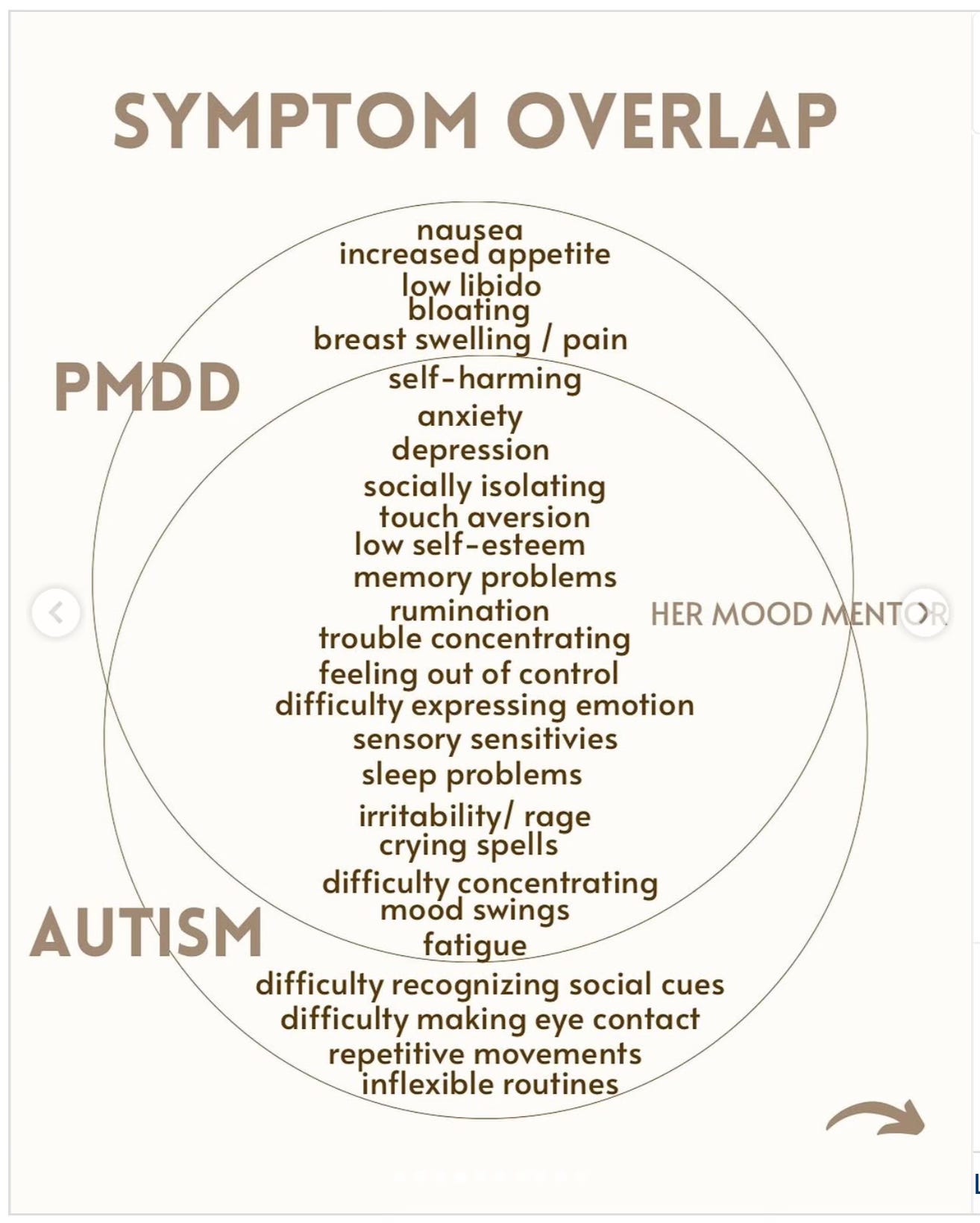
I love an infographic and you might enjoy this one too:
💕
PMDD Treatments
Look, friends, it is too late for me. I ain’t healing from this. I am on a heavily medicalised path because I do not have the capacity to save myself from this autistic perimenopausal ADHD brain fog PMDD hell-spiral.
Please don’t tell me I just need to think more positively.
So what can be done for us in PMDD following a medical treatment plan?
Depending on your own information processing capacity I have two sources for you.
If you have mental clarity right now, you might like to explore this IAPMD PDF resource that covers all current PMDD treatment options, with pros and cons and differing levels of efficacy and safety. It is presented in an informative table format.
Dr Lynsay Matthews (on The Happy Menopause podcast, surely that is an oxymoron?) summarises the evidence-based clinical four treatment categories for relieving PMDD. If you are short on time and/or capacity, listen from 22:30 ish for a treatment run through. I have summarised the treatments for you below, paraphrasing from the episode.
Four categories of PMDD treatment:
Anti-depressants are effective in 60% of cases (SSRIs - Fluoxetine, Paroxetine, Sertraline etc.) and can be taken only in the luteal phase (post-ovulation until onset of bleeding). Known as onset dosing.
Hormonal treatments such as hormonal birth control/contraceptives. Less effective due to individual differences. May be life changing for some, but causes suicidality in others.
Chemical menopause is a medicine (GnRH Analogues e.g. Zoladex) used to pause your menstrual cycle. Alleviates PMDD symptoms for many people giving them a break, and validates that symptoms are menstrual cycle related. Useful for people intolerant of previous treatment options. Requires add-back HRT to maintain bone density and offset cardiovascular risk. A short term option, providing relief and giving time to make a long term plan.
Bilateral salpingo-oopherectomy and total hysterectomy (surgical removal of both ovaries and uterus). Removes the source of the menstrual cycle and fluctuating hormones. Requires add-back HRT to protect from dementia, cardiovascular disease, osteoporosis. Drastic treatment option, but may be required by people facing monthly suicide attempts, self-harm.
💕
Shut this shit down
I have used the first three treatments and found some relief, but I am self-advocating for a surgical menopause. Personally I can no longer cope with the unpredictability of ongoing autistic perimenopause.
This week I had my first bleed since I started on hormone blockers to cause my chemical menopause, and it completely freaked me out. I immediately emailed my long suffering doctor who reassured me that this bleed was hormonal (it was preceded by debilitating menstrual cramps and a week of moderate depression) rather than a symptom of endometrial cancer as I had feared.
The thought of ever bleeding again is utterly sickening to me. It triggers sensory overload and reverts me into a state of unresolved pregnancy loss trauma.
Friends and family who have had hysterectomies often speak of them improving their quality of life, even when they didn’t have PMDD.
Several Auti Peri Q&A interviewees have shared that their surgical menopause gave them reprieve from their auti peri symptoms, even if they didn’t yet identify as neurodivergent.
Perimenopause worsens PMDD because we no longer have predictable cycles, and don’t know when the next “good week” might be. This can leave us bereft of any symptom relief, unable to make plans, feeling hyper vigilant and unsafe at all times.
It can destroy our relationships. Traumatise our children. Chronically dysregulate us. Make us feel bewildered and despairing.
Toxic positivity menopause messaging around this life phase is exclusive of our neurodivergent lived experiences. Positing perimenopause as being an opportunity to reinvent ourselves dismisses the horrors many of us face.
I was extremely reluctant to trial a chemical menopause. When I told my HRT doctor that I had read that some people say that if we lean into perimenopause and rest, then we can emerge post-menopausally ready for anything, she soon put me straight.
“Sam, from what I have observed of other patients like you, if we don’t treat this now you may feel like a shell of your former self after menopause.”
My HRT doctor is now my strongest advocate for my hysterectomy, but opinions can differ between professionals. Another doctor told me, when I described my symptoms and distress that:
“Sam, public gynaecology does not have time and resources for your problems".
Medical opinions can feel like polar opposites, and our suffering can all too easily be gaslit and dismissed.
Self-advocacy is vital. Menopausal awareness is imperative. And seeking neuroaffirming clinicians for second and third opinions is soul destroying fundamental.
Bonus tip: Yes, cats can help. Please accept this gallery of my pet floofs as a non-medical therapy option. Can you spot which photos I took through a tube for effect? 🧻









What’s the good news?
Post-menopause can liberate us from the hormonal fluctuations that trigger PMDD episodes due to our hormone levels decreasing and eventually flatlining. This means that we can hope for an improved quality of life in our later years.
However, we may experience residual trauma and psychological symptoms may have become long term behaviours beyond the menopause transition…
Are you dealing with PMDD at the moment, or have done in the past? I would love to know what you have found beneficial in the comments.
P.S.: Harry and Toby send their love! 🐾 🐾
















Share this post